Full Text
Introduction
Orbital cellulitis is a common life threatening infection of the postseptal tissues of the orbit and one of the common causes of orbital inflammation [1, 2]. It occurs most commonly in children and young adults [3]. Orbital cellulitis is an inflammatory disorder of the orbit. It is thought to occur as a result of an acute spread of infection from the blood, adjacent tissues, and facial skin [2].
Periorbital trauma and dental infection are other sources of spread to the orbit [2]. Most cases seen in the hospital and reported in texts are unilateral, only involving the second eye if the cavernous sinus is involved. Direct spread of the disease through the ophthalmic veins to the cavernous sinus and centrifugally to the contralateral orbit through the dura matter has been postulated as the mechanism of involvement of the orbit resulting in bilateral orbital cellulitis [4, 5].
Regarding the management of orbital cellulitis, the standard protocol includes immediate hospitalization with prompt empirical intervention targeting the likely causative organisms with respect to the age of the patient and the presenting history [2, 3]. Prior to medical therapy, a computerized tomography scan (CT scan) should be obtained and blood samples taken for full blood count analysis and blood culture [2, 3]. Purulent materials from the nose and eyes are also collected for microscopy, culture and sensitivity [3]. Magnetic resonance imaging is required to make a diagnosis of orbital abscess or determine cavernous sinus involvement [3].
Treatment is with broad- spectrum antibiotics and surgical drainage of subperiosteal or orbital abscess when required [2]. The patient stays admitted in the hospital and the intravenous medication continued until he is fever-free [3].
Case report
A 3-year-old male child presented to us with history of fever with chills and rigors, moderate grade, continuous in nature since 15 days. He developed pain, swelling and redness of left upper eyelid since 8 days, gradual in onset and progressed rapidly and child was unable to open the eye completely at the time of presentation since 3 days. Child complained of pain, swelling and restricted movements of left knee since 4 days. Child was irritable and not having regular feeds orally since 3 days. Previously, patient was admitted in outside hospital since last 1 week and was given intravenous antibiotics i.e., Ceftriaxone, Tazobactum and Amikacin. Investigations done in outside hospital are –WBC-21,000, CRP- 42.4, CUE- 4-6 pus cells, ASO titres-positive (1:2). Since there was no improvement patient was shifted to our tertiary care centre for further treatment. On general physical examination, patient was moderately built, moderately nourished, well oriented to time, place and person. His Temperature was 102oF, Pulse: 100/min, BP: 100/70 mm of Hg, RR: 20/min and SPO2-100% on room air. His systemic examination was normal. On ENT examination, left middle meatus showed purulent discharge. On Orthopaedic examination, movements were painful and restricted beyond 20o in left knee. His visual acuity was Fixating and following light. Child was not co-operative for testing extra ocular movements. On anterior segment examination there was diffuse upper lid edema of left eye associated with mild erythema and matting of lashes, left conjunctiva shows mild congestion. Fundoscopy done under sedation was normal.
Investigations: At the time of admission, Hb-10.2gm%; WBC count- 20,640 millions/cumm; polymorphs-76%; lymphocytes-16%; WBC-Neutrophilic leucocytosis and lymphopenia; ESR- 83 mm/hr.; CRP- 9.81 mg/dl.
CT joint/ limbs (plain) each region
CT scan of knee joint technique: CT study of left knee joint was performed on 128 Detector Row /Multislice CTscanner findings: Lower end of the femur and upper end of tibia, fibula and patella are normal. No obvious lytic/sclerotic lesion seen. No evidence of any fracture seen. Muscles around knee joint are showing normal attenuation.
PUS culture & sensitivity: Methicillin resistant Staphylococcus aureus (MRSA) grown in culture.
MRSA: Oxacillin resistant Staphylococcus aureus are resistant to all pencillin’s cephalosporins (except ceftobiprole). Betalactams/ Betalactamase inhibitor combinations and carbapenems.
MRI brain: Diffuse restriction in left maxillary and ethmoid sinuses. Abscess collection in superior and medial extraconal compartment of left orbit extending into preseptal space. T2/ FLAIR hyper intensitivity with diffusion restriction is noted in left ethmoid and maxillary sinuses? pyocele- likely extension of infection from left paranasal sinuses across lamina papyracea into extraconal and preseptal compartments of left orbit.
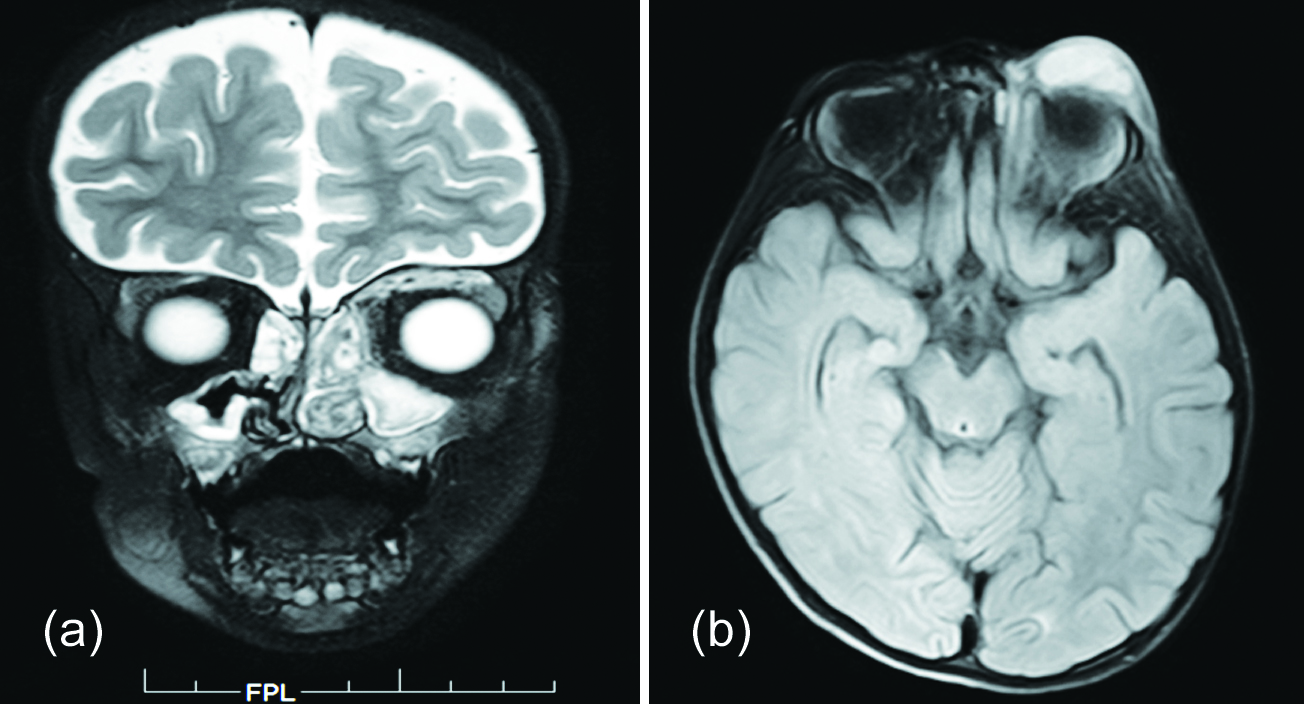
Figure 1: (a) T2 coronal section of MRI showing bilateral maxiallary and ethmoidal sinusitis with defect in lamina papyracea and collection in superomedial aspect of extraconal space. (b) T2 axial section of MRI showing collection of pus in left preseptal space.
Diagnosis
Based on the above examination and investigations, patient was diagnosed with left sided pansinusitis with orbital cellulitis and reactive arthritis of left knee.
Treatment
Functional endoscopic sinus surgery with orbital decompression was done under general anesthesia and continued on intravenous antibiotics (Figure 2a, b). Pus culture and sensitivity showed MRSA positive growth and child was continued on antibiotics i.e., Teicoplanin and Metrogyl for one week. Patient showed marked improvement in both ocular and general condition (Figure 3). Repeat investigations were suggestive of decreasing WBC count. TC-14600 millions/cumm; ESR- 69 mm/hr; CRP-4.43mg/dl.
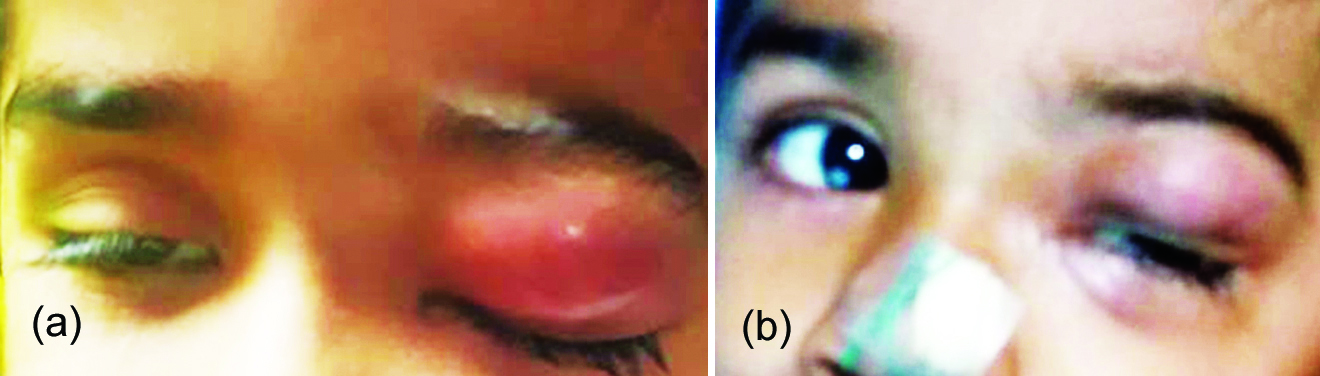
Figure 2: (a) Patient condition: At the time of admission. (b) After surgery - On Postoperative day 1.

Figure 3: Follow up- After 2 weeks.
Discussion
Infections of the orbit and periorbital tissues are important because they are life-threatening and therefore demand prompt, specific therapeutic management. These infections may spread through the dehiscence of the orbital bony wall or via the venous drainage of the orbit [6]. These veins, which characteristically have no valves, drain into the pterygoid plexus or the cavernous sinus [7]. The spread to the cavernous sinus may result in septic thrombosis and bilateral cavernous sinus infection, meningitis, or brain abscess [3]. The bilateral involvement of the cavernous sinus most frequently results in a contiguous spread to the contralateral orbit. This is the postulated pathway for the development of bilateral orbital cellulitis and it may be associated with altered consciousness if an intracranial abscess develops [3].
Orbital cellulitis has been associated with a number of serious complications including loss of visual acquity, cavernous sinus thrombosis, meningitis, frontal abscess, osteomyelitis and even death [8].
Specifically in pediatric population, up to 90% of patients with orbital cellulitis had existing sinusitis, with almost half having multiple sinus involvement. After sinusitis, periocular trauma and history of ocular or periocular surgery were the cause of significant number of cases of orbital cellulitis among the patients [8, 9]. Less commonly reported causes of orbital cellulitis such as dacrocystitis, dental infection, and endophthalmitis also were found among the patients. Sinusitis may also produce osteomyelitis and intracranial abscess. Osteomyelitis commonly involving the frontal bone is a direct extension of frontal infection or septic thrombophlebitis via the valveless sinus of Breschet. Osteomyelitis is rare in the ethmoids because from this location, infection can rapidly spread through the thin lamina papyracea into the orbit or maxillae, where arterial anastamoses are sufficient to prevent necrosis due to septic thrombosis of a single artery. Although, meningitis is the most common intracranial complication of sinus disease, epidural, subdural, and brain parenchymal abscess can occur [10].
The index child in the report presented 15 days after onset of symptoms. He was febrile and irritable with painful swelling of left eye with rhinorrhea and left knee. He, however, had rhinorrhea prompting a working diagnosis of orbital cellulitis secondary to rhinosinusitis [11].
The most common complication of rhinosinusitis in children is orbital cellulitis. Others with increasing severity include subperiosteal abscess, intraorbital abscess, and cavernous sinus thrombosis [11]. The ethmoidal sinus is the most common source of infection in children, as the frontal and sphenoidal sinuses do not develop until age 7 [12]. Radiological investigations, particularly CT scan and MRI, are keys to the diagnosis of orbital disorders and show clearly the changes occurring within the orbit [4].
Clinically, orbital cellulitis presents with pain, proptosis, globe displacement, double vision and/or vision loss, chemosis, and extraocular motility deficit (ophthalmoplegia). Patients will often have accompanying headache and malaise. In children, fever occurs with equal incidence as in preseptal cellulitis (62%) [13] while it may be absent in adults 66% of the time [14].
Antecedent and significant past medical history may include a history of headache, rhinitis, sinusitis, nasal discharge, and recent upper respiratory tract infection. Decreased visual acuity, pupillary signs, and vision loss may occur rapidly. Optic neuropathy and optic disc edema may be observed.
In bilateral cases as noted in orbital cellulitis classifications, all the above feaures become more marked and bilateral due to the involvement of the cavernous sinus [11]. The index child presented with most of the clinical features listed above but had no altered sensorium. A retrospective review of orbital cellulitis complicating sinusitis showed a preferential involvement of the left orbit in 55% of the cases [15].
The authors believe that the left eye involvement was as a result of a direct spread to the left orbit through the ipsilateral ethmoidal sinus.
The relatively early presentation of the patient with the timely institution of empirical treatment based on the organisms usually implicated in childhood orbital cellulitis may have limited the effects in the left eye. In children, Haemophilus influenza, Staphylococcus aureus, Streptococcus species, and anaerobic organisms were implicated as the commonest causes of orbital cellulitis in descending order of frequency of bacteria organisms [16]. However, recent studies have shown that S. aureus and Streptococcus species have been implicated in most cases of preseptal or orbital cellulitis [15]. It is important to note that sinoorbital infections do not always respect the guidelines, and orbital cellulitis with a potpourri of organisms has been reported in case reports and series [14].
However, it has been reported that blood culture, and sensitivity, though important, usually yields no growth; rather, the swabs taken endoscopically from the paranasal sinus yield better results [17, 18].
Generally, the duration of treatment depends on the patient’s response. Patients should be treated parenterally until they show signs of clinical improvement. The index child showed no clinical improvement even after treatment with parenteral and topical antibiotics in outside hospital. The patient started showing improvement only after surgical drainage of abscess and administration of antibiotics based on culture sensitivity report of pus drained during surgery. Patient was discharged after 8 days stay in the hospital on oral drugs. Other studies have reported an average hospital stay of 15 days with a range of 10-25 days [5, 13].
Surgical treatment is indicated for significant underlying sinus disease, orbital or subperiosteal abscess or both in the paediatric age group. Urgent drainage, usually within 24 hours, is indicated for the following: large orbital abscess causing discomfort, superior or inferior orbital abscess, evidence of intracranial extension, involvement of frontal sinuses, and a known dental source of the infection in patients older than 9 years [19].
Indications for surgical intervention include persistent localized collection without clinical improvement, increasing proptosis with systemic sepsis, fulminant sinusitis with impaired drainage, and when foreign bodies are suspected [20].
Conclusion
Orbital cellulitis is more common in children and young adults, typically from an acute or acute on chronic sinusitis. Medical management remains the mainstay of treatment in preseptal and orbital cellulitis. Surgical drainage of the abscess is considered when the infection progresses or does not respond to medical management or threatening vision. In MRSA infections, first line of treatment is Piperacillin with Tazobactum or Ertapenem with clindamycin. When patient is not responding to first line of treatment, then next line of treatment is Teicoplanin or Vancomycin as monotherapy. Metronidazole is used for the treatment of infections caused by anaerobic organisms.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Wulc AE. Orbitalinfections. In: Linberg J, editor. Duane’s Ophthalmology. CD-ROM ed, clinical vol 2. Philadelphia: Lippincot Williams and Wilkinson; 2002. Chapter 34.
[2] Kanski JJ. Orbit in Clinical Ophthalmology. 5th ed. Edinburgh, New York: Butterworth Heinemann. pp 568–9.
[3] Harrington JN. Orbital Cellulitis. Accessed on 3 Dec 2015 from: http://emedicine.medscape.com/article/1217858
[4] Eustis HS, Mafee MF, Walton C, Mondonca J. MR imaging and CT of orbital infections and complications in acute rhinosinusitis. Radiol Clin North Am. 1998; 36(6):1165–1183.
[5] Singh SK, James E, Sabarigirish K, Swami H, Sood T. Bilateral orbital complications of paediatric rhinosinusitis. Med J Armed Forces India. 2014; 70(1):68–72.
[6] Harris G. Subperiosteal abscess of the orbit. Arch Ophthalmol. 1983; 101(5):751–757.
[7] Batson OV. Relationship of the eye to the paranasal sinuses. Arch Ophthalmol. 1936; 16:322–323.
[8] Ferguson MP, McNab AA. Current treatment and outcome in orbital cellulitis. Aust N Z J Ophthalmol. 1999; 27(6):375–379.
[9] Jarrett WH, Gutman FA. Ocular complications of infection in the paranasal sinuses. Arch Ophthalmol. 1969; 81(5):683–688.
[10] Hornblass A, Herschorn BJ, Stern K, Grimes C. Orbital abscess. Surv Ophthalmol. 1984; 29(3):169–178.
[11] Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970; 80(9):1414–1428.
[12] Mitchell R, Kelly J, Wagner J. Bilateral orbital complications of paediatric rhinosinusitis. Arch Otolaryngol Head Neck Surg. 2002; 128(8):971–974.
[13] Schramm VL Jr, Curtin HD, Kennerdell JS. Evaluation of orbital cellulitis and results of treatment. Laryngoscope. 1982; 92 (7 Pt 1):732–738.
[14] Bergin DJ, Wright JE. Orbital cellulitis. Br J Ophthalmol. 1986; 70(3):174–178.
[15] Nwaorgu OG, Awobem FJ, Onakoya PA, Awobem AA. Orbital cellulitis complicating sinusitis: A 15-year review. Nig J Surg Res. 2004; 6(1-2):14–16.
[16] Morgan PR, Morrison WV. Complications of frontal and ethmoid sinusitis. Laryngoscope. 1980; 90(4):661–666.
[17] Georgakopoulos CD, Eliopoulou MI, Stasinos S, Exarchou A, Pharmakakis N, Varvarigou A. Periorbital and orbital cellulitis: A 10-year review of hospitalized children. Eur J Ophthalmol. 2010; 20(6): 1066–1072.
[18] Kamath MP, Shenoy SV, Mittal N, Sharma N. Microbiological analysis of paranasal sinuses in chronic sinusitis − A south Indian coastal study. Egypt J Ear Nose Throat Allied Sci. 2013; 14(3):185–189.
[19] Harris GJ. Sub periosteal abscess of the orbit: age as a factor in the bacteriology and response to treatment. Ophthalmology. 1994; 101(3):585–595.
[20] Bedwell J, Bauman NM. Management of pediatric orbital cellulitis and abscess. Curr Opin Otolaryngol Head Neck Surg. 2011; 19(6):467–473.