Full Text
Introduction
In daily radiological practice, one often encounters problems in differentiating real bone tumors from tumoral bone lesions. Bone reacts in limited ways for any stimulus of developmental or acquired nature. These pathological reactions are reflected in radiology and imaging investigations. These include new or reactive bone which is dense, lysis of the bone are non-mineralized matrix which is lucent and periosteal reaction in several patterns. It may be a combination of these lesions. Conventional radiology is often adequate to diagnose tumoral lesions of bone, without further imaging studies. Tumoral lesions of bone are of several types which are mentioned in table I. These lesions pose a diagnostic problem but can be differentiated from tumors by detailed study. This review attempts at solving these problems by studying the radiological findings in each entity. However, many of these radiological findings should be evaluated in the light of clinical setting where age is an important factor. The common tumoral lesions are listed in table I
Table 1: The common tumoral lesions.
|
Bone islands
Fibro osseous lesions - Ossifying fibroma, osteofibrous dysplasia, fibrous dysplasia
Fibrocortical defects
Non-ossifying fibroma
Simple bone cyst (SBC)
Aneurysmal bone cyst (ABC)
Post traumatic bone lesion
Dystrophic calcification / Ossification
Granulomas – Histiocytosis X & sarcoid
Infective lesions – Bacterial, fungal
Pseudotumor hemophili
Pseudotumor gout
Brown tumor
Bone infarct
Intraosseous ganglion
|
Bone islands
These are often encountered as circumscribed homogenous dense lesions on plain films. The size may range from few millimetres to a centimetre and may simulate osteoid osteoma which has typical radiological findings such as a nidus and surrounding reaction (Figure 1ab). It may grow and assume a large size when it is called a giant bone island (Figure 1c). Developmentally, these bone islands are cortical inclusions in trabecular bone. They may be multiple and involve many bones, and should not be mistaken for osteopoikilosis (Figure 1d).
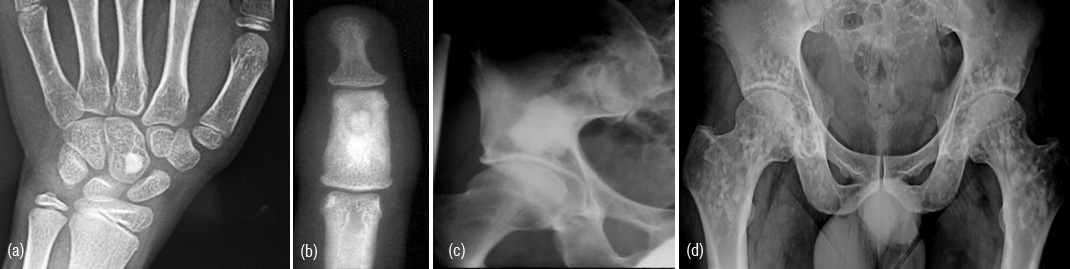
Figures 1a,b,c,d: a) Bone island in capitate, b) Osteoid osteoma, c) Giant bone island in iliac bone, d) Osteopoikilosis.
Fibro osseous lesions
Ossifying fibroma
It may be encountered in childhood, from infancy to 10 years of age. Radiologically, it is a lytic lesion with multiloculated sclerotic borders. Anterior bowing of the tibia is a common feature (Figure 2ab). Spontaneous regression is well known and is often called a “leave me alone lesion”. However, subsequent to trauma or surgery, pseudo arthrosis may develop. It may also occur in the bones of the jaw.

Figure 2a,b: Ossifying fibroma of the tibia.
|
|
Ossifying fibroma
|
Fibrous dysplasia
|
|
Age & radiological features
|
0-10 yrs
lytic expanding Intramedullary
lesion with cortical involvement
|
Any age
lytic expanding
lesion with ground glass matrix
|
|
Site
|
Mid shaft
|
Any part of the bone
|
|
Complications
|
Pseudo arthrosis
Spontaneous regression
|
Rare
Not known
|
Some authors consider ossifying fibroma and osteofibrous dysplasia as a spectrum of the same entity.
Osteofibrous dysplasia
It is also named as Kempson-campanacci lesion. It commonly involves tibia shaft. Radiologically, an elongated lytic lesion with areas of sclerosis and anterior bowing (Figure 3abc).
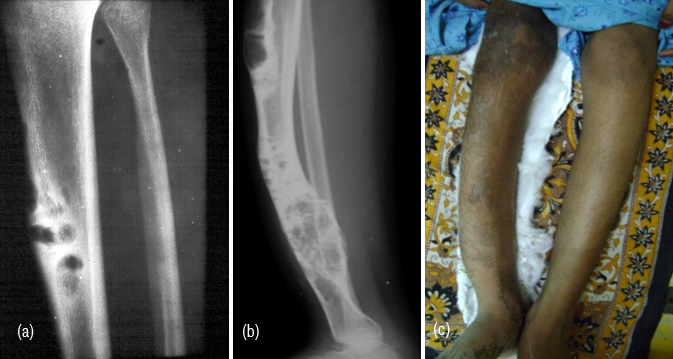
Figure 3: (a) osteofibrous dysplasia involving mid tibia. (b, c) 14-year-old girl - Osteofibrous dysplasia involving the entire tibia.
Fibrous dysplasia
Most common bone dysplasia where fibrous aberration occurs replacing the bone as a developmental error. A defective gene exists in the cells that form bone and other tissues. It may be monostotic and may simulate a benign or malignant bone tumor. However, the radiological features such as transitional zone in an expanding lytic area, thick sclerotic rind, ground glass appearance of the matrix and local deformity of bone differentiate from benign bone tumors (Figure 4abcd). On rare occasions chondroid type of calcifications may be seen. Pathological fractures may occur and the lesion may be aggressive simulating malignancy.
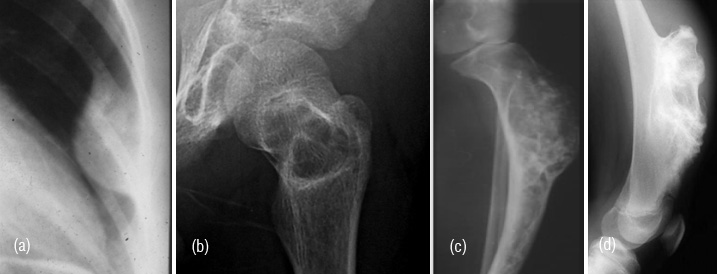
Figure 4: (a) Fibrous dysplasia of rib, (b) neck of femur with pathological fracture, (c) aggressive lesion simulating cartilagenous lesion, (d) Sessile exostosis simulating fibrous dysplasia.
Fibrous cortical defects
Fibrous cortical defects are developmental errors where periosteal membrane is included in the cortex of the long bones (Figure 5). It is encountered in children and spontaneous resolution is known. On the other hand, they may progress to non-ossifying fibroma.

Figure 5: Large fibrous cortical defect.
Non ossifying fibroma
These are cortical oriented fibrous lesions often encountered between 12 and 30 years. Lower limb bones are most commonly involved. Radiologically, a large, oblong lytic lesion with sclerotic borders (Figure 6ab). The patient clinically presents with a pathological fracture. In the healing phase, new bone forms from the periphery (Figure 6c).

Figure 6: (a, b) Non-ossifying fibroma involving lower end of tibia, (c) Healing non-ossifying fibroma.
Simple bone cyst (SBC)
It is also named as unilocular bone cyst encountered in children and young adults in long bones. Radiologically, it is vertically expanding lytic lesion with thin transitional zone in the metaphyseal area which may extend to diaphysis. Several septae may be seen and pathological fracture is not uncommon. A fallen fragment sign is classical for radiological diagnosis of simple bone cyst. This is well demonstrated in erect and supine or horizontal beam films (Figure 7ab). A simple bone cyst is occasionally seen in adults particularly in the calcaneum, iliac and other bones (Figure 7cd). This may simulate lytic metastasis (Figure 7e). Brodie’s abscess/ tubercular abscess may also simulate (Figure 7f).
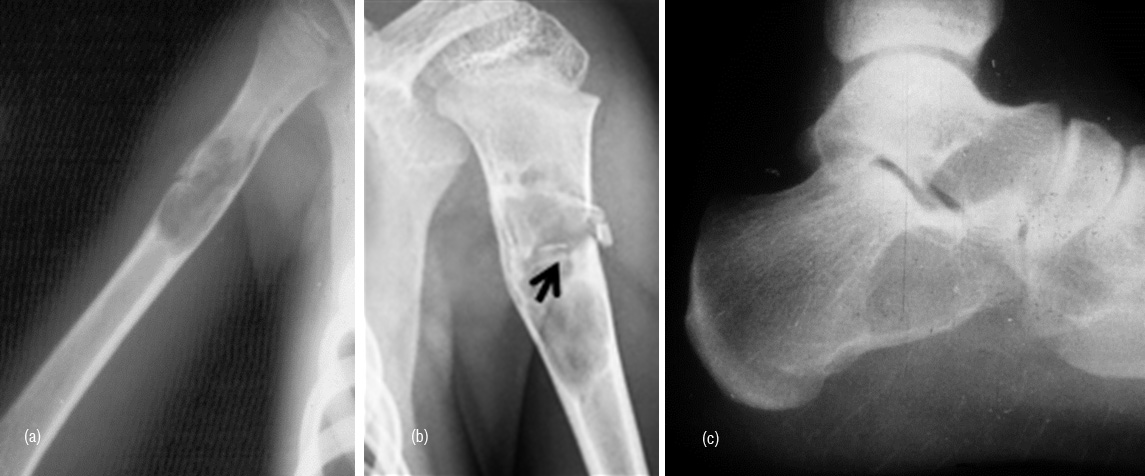
Figure 7: (a) SBC with fracture, (b) Fallen fragment (arrow), (c) SBC in calcaneum.
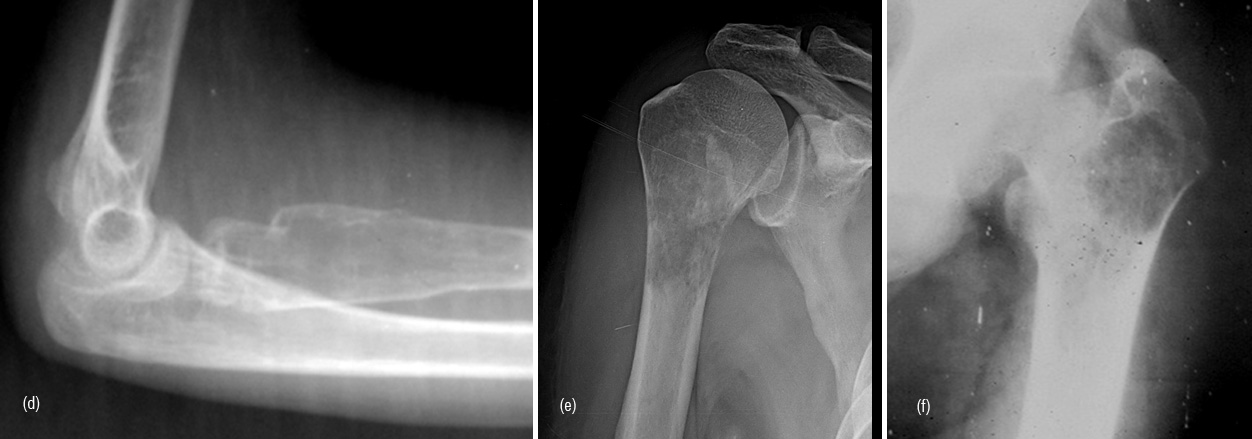
Figure 7: (d) SBC in radius, (e) Metastasis from bronchogenic carcinoma, (f) Tuberculous abscess.
Aneurysmal bone cyst (ABC)
It may be primary or secondary. Secondary ABC is associated with giant cell tumor, chondroblastoma, chondromyxoid fibroma, fibrous dysplasia, osteoblastoma, ewings tumor and telangiectatic osteosarcoma.
Primary ABC is radiologically an expanding lucent lesion with thin transitional zone located in diametaphyseal or diaphyseal area. It is encountered generally in young age but it also may be seen in adults. Pathological fractures may occur. A thin shell of bone is often noted (Figure 8abc). In spine, it may involve the body/pedicle/spinus process of vertebra (Figure 8d). In CT/MRI fluid fluid levels may be noted (Figure 8e). However, fluid fluid levels may also be seen in other lesions such as giant cell tumor. A solid variety of ABC is also seen and pathologists consider this as a variant of giant cell reparative granuloma which often occurs in the bones of hand and face.
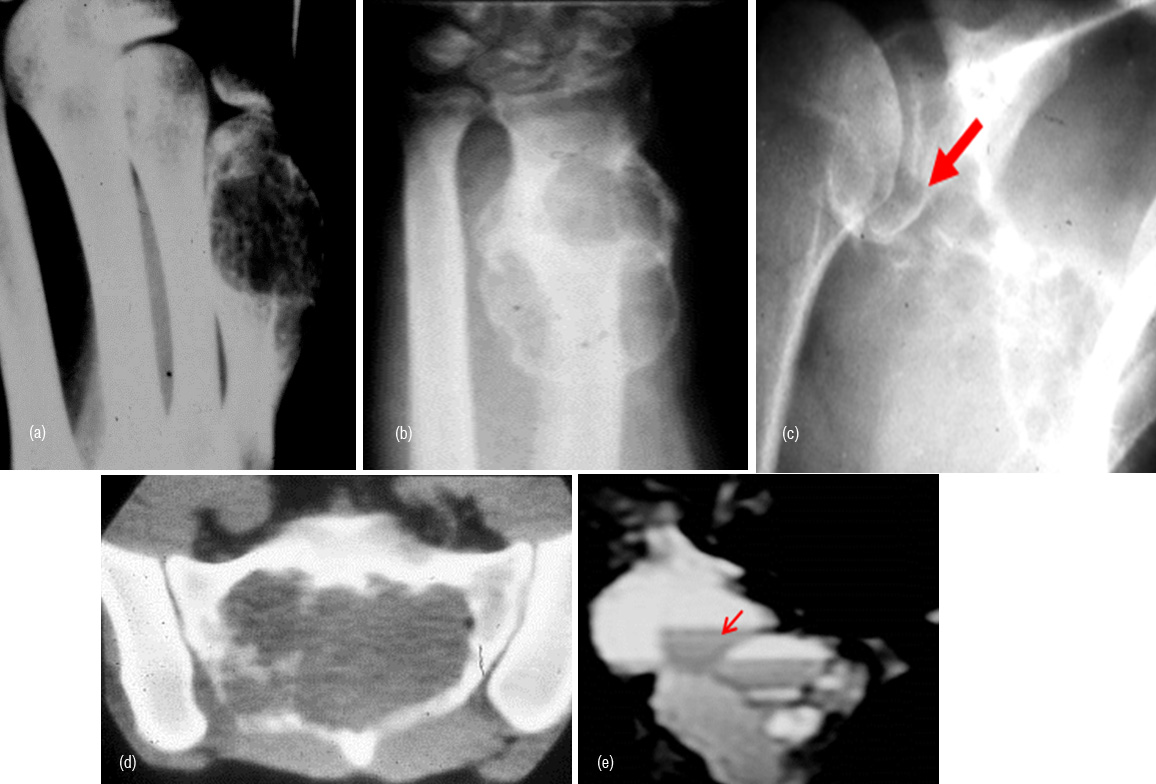
Figure 8: ABC, (a) 5th metacarpal, (b) Radius, (c) Scapula, (d) Sacrum may simulate giant cell, (e) Fluid fluid levels in ABC (MRI).
Post traumatic bone lesion
In avulsive lesions of apophysis, the healing phase of the lesion simulates a bone tumor such as pariosteal osteosarcoma (Figure 9ab). This is due to abundant callus and associated calcified hematoma with myositis ossificans. These lesions are well circumscribed without any soft tissue swelling. If one is not familiar with this entity, these may be mistaken for benign or malignant osteogenic tumors. Post traumatic myositis ossificans can occasionally simulate osteochondroma or other benign bone lesion (Figure 9cde). In a bedridden patient due to neurological cause’s dystrophic calcification/ ossification is commonly encountered in the soft tissues particularly in pelvic region which may be mistaken for an osseous tumor such as pariosteal osteosarcoma (Figure 9f).
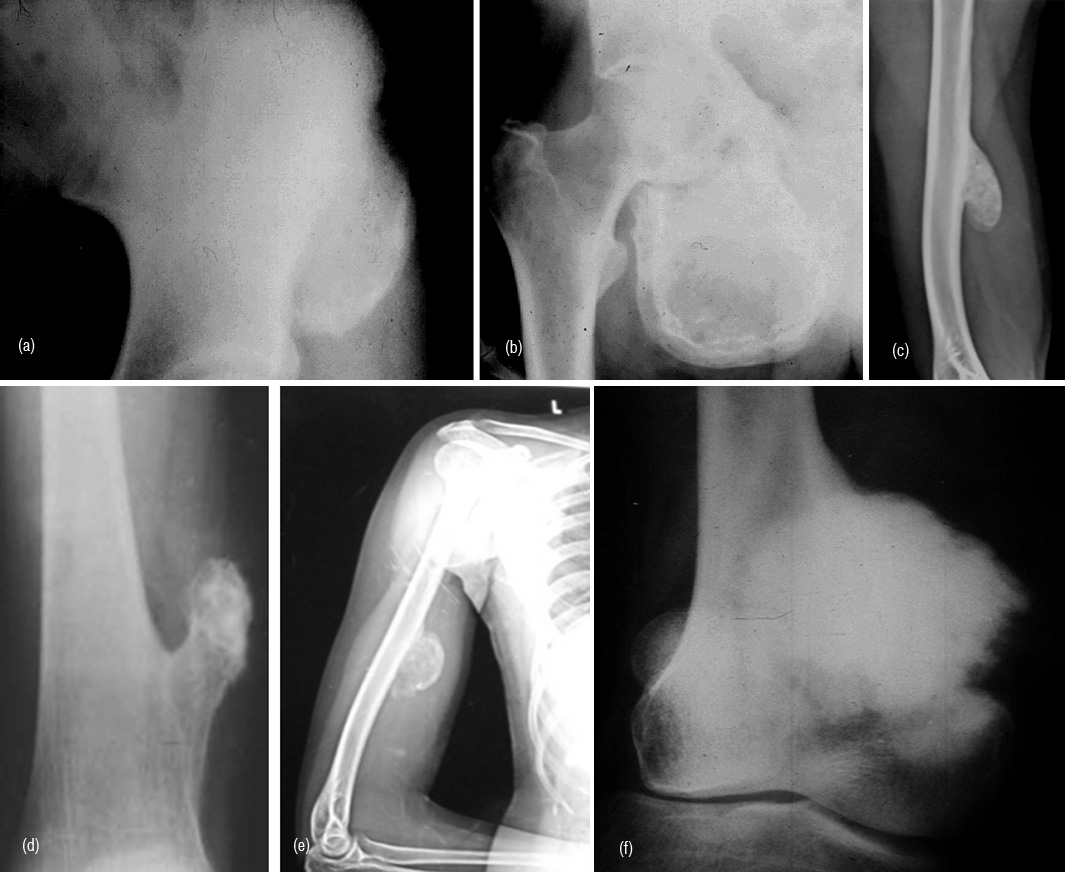
Figure 9: (a) Avulsion injury at the attachment of rectus femoris to anterior inferior iliac spine, (b) Avulsion injury of the adductors to ischial apophysis. Note the abundant callus and myositis ossificans. (c) Post traumatic myositis ossificans, (d) Exostosis, (e) Myositis ossificans, (f) Pariosteal osteosarcoma.
Dystrophic calcification/ ossification
It occurs in patients with spinal cord injury or other neurological disorders. Excessive granulation tissue leads to fibroblastic proliferation leading to osteocytic activity (Figure 10a,b).
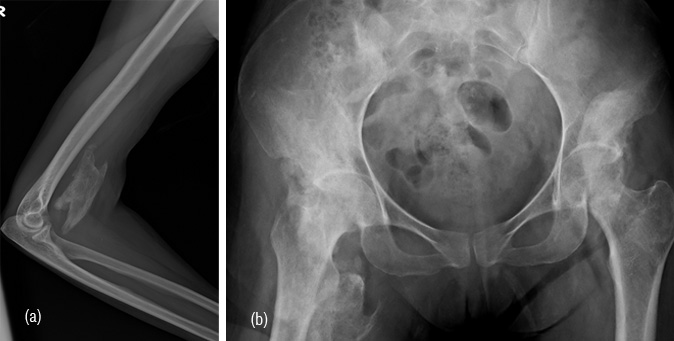
Figure 10: (a) Dystrophic ossification in bedridden patient, (b) Soft tissue ossifications in a patient with paraplegia.
Granulomas
Langerhan’s histiocytosis X is commonly encoutered in children. However, a solitary lesion eg., eosinophilic granuloma may also be seen in adults. Radiologically, eosinophilic granuloma is a solitary lytic lesion in the medulla of a long bone with endosteal scalloping. It may break the cortex and produce periosteal reaction (Figure 11a). When lytic it may simulate metastasis (Figure 11b). In the skull, the edges of the lytic lesion may have a bevelled edges (Figure 11c). In Hand Shuller Christian type of histiocytosis which is encoutered in young adults associated with enlargement of liver and spleen, bone lesions are multiple and may simulate lymphoma or metastasis (Figure 11d).
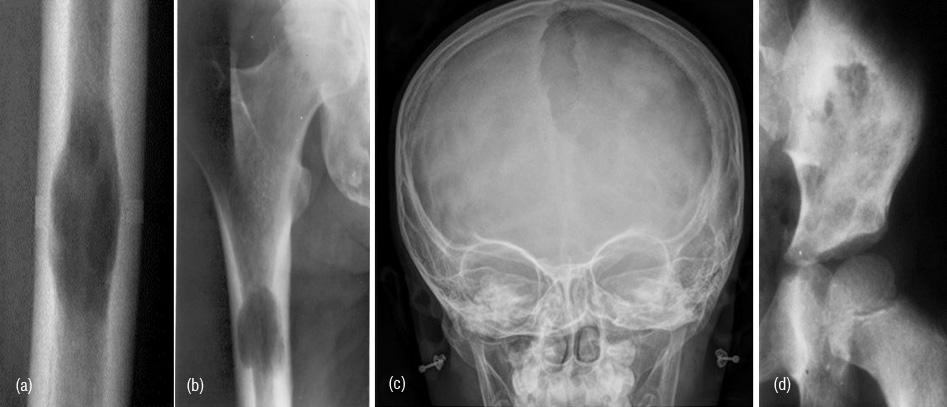
Figure 11: (a) Eosinophilic granuloma in femur, (b) Metastasis from bronchogenic carcinoma, (c) Large eosinophilic granuloma in skull, (d) Langerhan’s histiocytosis X in iliac bone with multiple lytic lesions.
Sarcoid
Sarcoidosis involving the bones is quite rare. However, lytic lesions in the bones of hands are more common than sclerotic lesions in the skeleton.
Infective lesions – bacterial, fungal
Inspite of introduction of several antibiotics, osteomyelitis, specially of long bones is still encountered. Brodie’s abscess a form of subacute bacterial osteomyelitis may resemble a neoplasm. Radiological characterists include an oval or elongated lucent lesion in the metaphysis with sclerotic border. A small sequestrum may be occasionally noted along with minimal periosteal reaction (Figure 12a,b,c).

Figure 12: (a, b) Brodie’s abcess in the lower end of tibia with minimal sclerosis along the border, (c) Brodie’s abscess along with periosteal reaction in the lower end of tibia.
Tuberculosis
Tuberculosis (TB) of the bones is less common than joint tubeculosis. Cystic type of tuberculosis may be confused for a bone tumor. Radioloigcal characteristics are almost the same as Brodie’s abscess. However, reactive new bone and periosteal reaction is minimal (Figure 13ab). Clinical and laboratory details will establish the diagnosis.

Figure 13a,b: TB abscess of lower end of tibia.
Fungal infections
Infections from nocardiosis, madura mycosis and aspergillosis rarely resemble osteoid osteoma and other tumors. These are chronic and indolent and produce various type of periosteal reaction and reactive sclerosis (Figure 14ab). When a lucent lesion with reactive sclerosis is noted, it may simulate osteoid osteoma (Figure 14c).
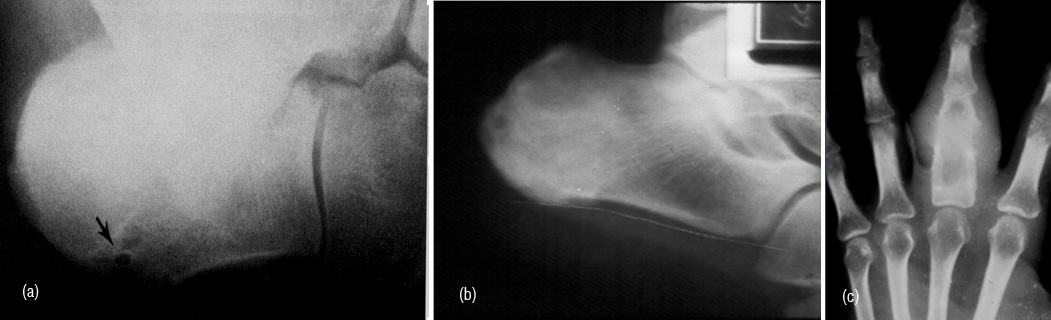
Figure 14: (a) Osteoid osteoma, (b) Fungal infection, (c) Fungal infection.
Pseudotumor hemophili
Hemophilic patients at times present a cystic lesion filled with blood as a rare complication. Repeated intraosseous bleeding produces a well defined uni or multilocular lytic expanding lesion. These are located either in metaphysis or epiphysis (Figure 15).

Figure 15: Pseudotumor hemophili with large lucent multilayered lesion in the iliac bone.
Pseudotumor gout
Intraosseous gouty lesions in the foot at times may simulate a tumor. However, adjacent erosions and tophi render a clue to diagnosis (Figure 16).

Figure 16: Intraosseous gout simulating a tumor.
Brown tumor
Brown tumors (BT) are areas hemorrhage with fibroblasts and osteoclasts encoutered in hyperparathyroidism both in primary and secondary. These are cortically oriented osteolytic lesions occuring anywhere in the skeleton but common in long and flat bones (Figure 17a). Histiologically, resemble osteoclastoma (Figure 17b).

Figure 17: (a) Brown tumor in ulna, (b) Giant cell tumor.
Bone infarcts
Old healed infarcts in the metaphyseal region of long bones simulate enchondroma. However, the radiological findings of an elongated lesion with serpentine calcifications and the peripherial fibroosseious membrane differentiates it from enchondroma (Figure 18abc). Occasionally the appearance may be similar to osteosarcoma (Figure 18d).
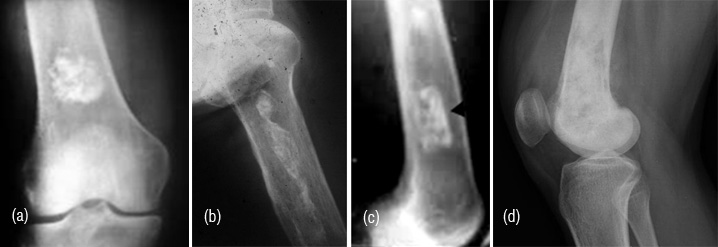
Figure 18: (a) Enchondroma, (b) Calcified infarct, (c) Calcified infarct in lateral view, (d) Osteosarcoma simulating infarct.
Intraosseous ganglion
It is a subarticular lytic lesion containing synovial fluid and is often associated with degenerative joint disease. It is encountered in the proximal and distal ends of tibia. Medial malleolus is common site (Figure 19).

Figure 19: Intraosseous ganglion in the medial condyle of tibia.
Conclusion
Bone reacts in a limited way and radioloigcally produces a sclerotic, lytic and a combination of these with variable periosteal reactions. Many sclerotic and lytic lesions encountered in the long bones in daily practice pose a problem differentiating benign bone tumors from tumoral lesions. These lesions should be carefully evaluated with further imaging correlating with clinical details. Occasionally, when they are aggressive may simulate primary malignant neoplasms. The varieties of tumoral lesions mimicing neoplasms are illustrated.
Acknowledgements
Acknowledgements are due to Department of Radiology and Imaging, KIMS, Secunderabad.
Conflict of interest
The author declares no conflict of interest.