Full Text
Introduction
Lumbar radiculopathy can be described as low back pain radiating to one or both lower extremity. The level of spinal nerve root involvement indicates specific dermatomes affected. Radicular pain and nerve root pain can occur as a single symptom (pain) that can arise from one or more spinal nerve roots [1]. Lumbar disc herniation contributes 60-80% of lifetime incidence of low back pain in general population [2]. Lumbar radiculopathy has an incidence of 23.09% in India [3, 4]. Many physical therapy interventions have been used to treat low back pain due to lumbar radiculopathy including traction, stretching, strengthening exercises, warm water fermentation, modalities like IFT but with varying degrees of success [5-7]. Though there are numerous treatments for lumbar radiculopathy, no single intervention has been proven to be most efficient. Brian Mulligan’s principle is based on “positional fault” [8]. In Mulligan’s spinal mobilization with limb movements (SMWLM’s) three therapist technique a sustained transverse glide is applied to the spinous process of specific spine while the restricted lower extremity movement is done simultaneously actively or passively.
Due to peripheral nerve compression the ability of the nerve to stretch and slide may be disrupted. Prolonged compression creates sequelae of intraneural events that may ultimately lead to impaired nerve sliding [9]. Neural mobilisation uses the Sliding Principle which was introduced by Shacklock, which consists of alteration of combined movements of two joints. These techniques aim to restore neural plasticity and lengthen the nerve bed by sliding the nerve. Neural tissue mobilization targets breaking adhesions in the structures present along the course of the nerve at the mechanical interface while the Mulligan concept corrects the positional fault at the spine. The effectiveness of these technique and clinical appropriateness is immediate reduction in pain and increase in mobility [10]. Studies have been conducted measuring the efficacy of Shacklock neural tissue mobilization and mulligan’s spinal mobilization with leg movement separately. No studies have been conducted combining both the techniques.
Methods and study design
90 subjects were recruited from Physiotherapy out-patient department, Nizam's Institute of Medical Sciences, Hyderabad, India. Subjects with subacute and chronic low back pain with unilateral lumbar radiculopathy who were diagnosed with disc bulge, protruded/ prolapsed intervertebral disc were included in the study.
Inclusion criteria: Age of 20-55 years of both sexes, unilateral radiculopathy in the distribution of specific nerve with positive straight leg raise (SLR), positive slump test of specific nerve bias of lumbar region, positive prone knee bend test, mild to moderate pain on a scale of NPRS < 7, hypaesthesia in specific dermatome of unilateral lower limb and impaired deep tendon reflex (knee jerk, ankle jerk).
Exclusion criteria: Subjects diagnosed with rapidly progressing neurological symptoms, extruded disc, dementia or other cognitive impairment, inflammatory or other specific disorders of spine such as ankylosing spondylitis, paget’s disease, vertebral collapse, rheumatoid arthritis, spondylolisthesis, severe osteoporosis, Tb spine, intermittent claudication, diabetic neuropathy, stenosis, sacroiliac joint pathology, previous spinal surgery, previous spinal injury causing radiculopathy, pathology of hip, knee and ankle and patient with known pregnancy and severe pain (NPRS > 7). More than one nerve root involvement, muscular involvement such as Piriformis syndrome, Red flags such as trauma, cancer, constitutional symptoms (fever, malaise, weight loss), recent infection, mental retardation, hemiparesis / hemiplegia.
The subjects were randomly assigned into three groups by lottery method who met the inclusion and exclusion criteria. Institutional Ethical Committee approval was taken. The allocations were concealed from the principal investigator. The outcome measures were single blinded and were taken by a physical therapist who was trained in taking the outcome measures. Informed consent was obtained from patient who met the criteria. Outcome measurements were Numeric Pain Rating Scale (NPRS) for pain intensity [11-13], Hip ROM during SLR- Universal Goniometer [14], back specific disability scores-Modified Oswestry Low Back Pain Questionnaire (MOLBPQ) [15]. Pre-treatment evaluation was done at the first day as baseline measurement. Group 1 included conventional therapy, Group 2 included neural tissue mobilization (NTM) and conventional therapy, Group 3 included Spinal mobilization with leg movement (SMWLM) three therapist techniques along with NTM and conventional therapy (Figure 1). At the end of session (zero day), the subjects were assessed for any increase in pain. If, no, adverse response was reported, further sessions were carried out. There were four dropouts. At six weeks final readings of all outcome measures were taken and data analysis was done for final results.
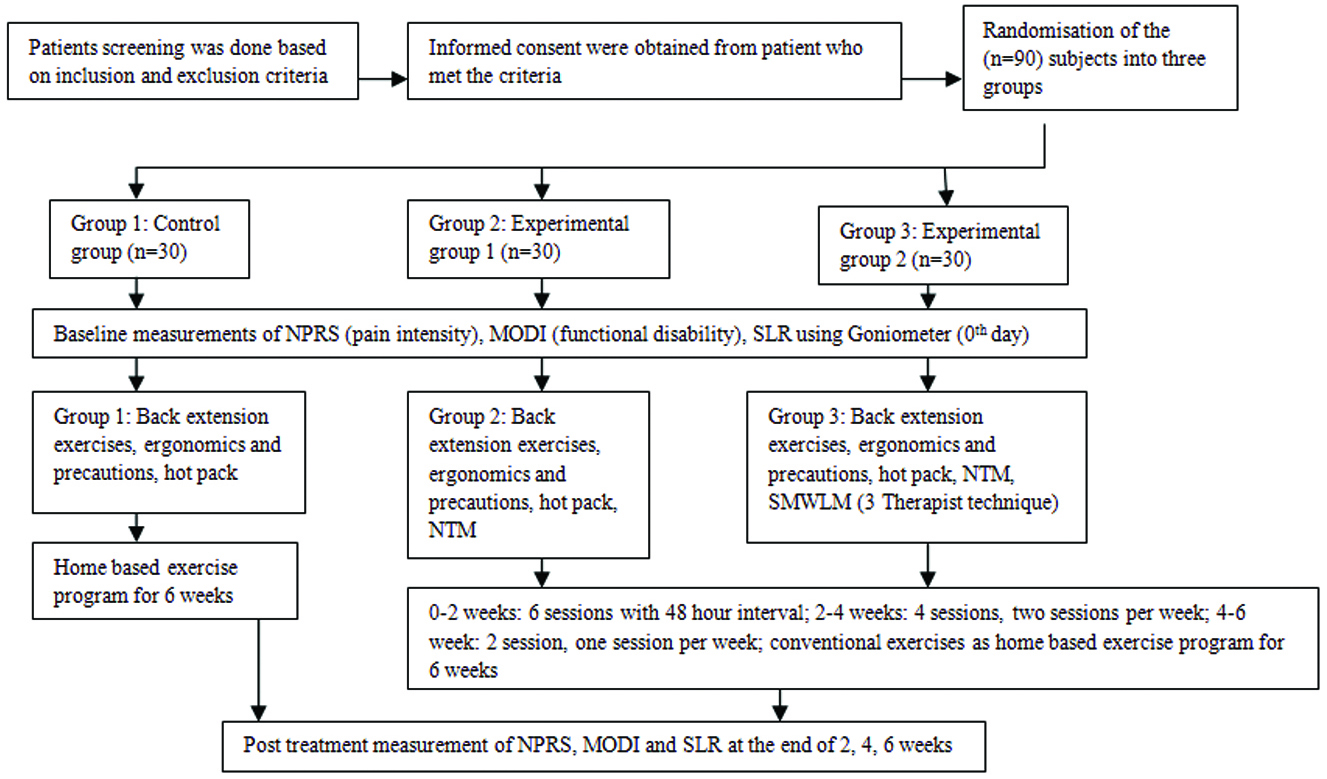
Figure 1: Consort flow chart of study.
Group 1 conventional therapy
Subjects received exercises which included back extension exercises: hyper extension of back (prone), hyper extension of back and flexion (kneel), extension opposite arm and leg [16], transverse abdominus contraction with pelvic floor muscle activation, superficial moist heat (hot pack) for 10 min, precaution and ergonomic advice [17]. These exercises were given as home programme to the subjects.
Dosage: 5 sets × 10 repetition with 2 min rest between each set for six weeks [18].
Group 2 neural tissue mobilisation and conventional therapy
Neural tissue mobilization was performed according to the norms/ guidelines by NDS, Australia [19]. Step 1- Sliders: Using unaffected joint (remote sequence, remote sliders). Affected joint is placed in neutral or symptom free position. Step 2- Sliders: Using unaffected joint (remote sequence, remote slider). Affected joint if placed some ROM but with or without minimal symptoms. Step 3- Sliders: (remote sequence, local sliders). Move affected area and any other area but with or without minimum symptoms.
Dosage: 30 sec to 2 min × 5 sets. Three days per week for two weeks. Two days per week from 2-4 weeks. One day per week from 4-6 weeks. Conventional therapy was given as home program to patients.
Group 3 SMWLM – 3 therapist technique, NTM & conventional therapy
SMWLM was performed according to norms/ guidelines by Mulligan's concept.
Dosage: Three set × 7 to 10 reps three days per week for two week. Two days per week from 2-4 weeks. One day per week from 4-6 weeks. Neural tissue mobilisation and conventional therapy was given as home program.
Results
Pain
There was no significant difference among control group, experimental group 1 and experimental group 2 on day 1 since f-value is 0.220 and P- value 0.803 is more than 0.05 (Table 1) (Figure 2). A significant difference exists among control group, group 1 and group 2 at week 2, 4, 6 since P-value 0.000 is less than 0.05. Since the paired t-test values of day 1 versus week 6 in control group, experimental group 1 and experimental group 2 are 12.776, 19.501 and 33.899 respectively and mean difference is more in experimental group 2 (Table 2). Hence there is significant improvement in pain reduction in the experimental group 2 when compared to experimental group 1 and control group.
Table 1: ANOVA test is used to test the significant mean difference between the groups of NPRS.
| |
|
Sum of squares
|
df
|
Mean square
|
F
|
Significance
|
|
NPRS day 1
|
| |
Between groups
|
0.309
|
2
|
0.154
|
0.220
|
0.803
|
| |
Within groups
|
58.215
|
83
|
0.701
|
|
|
| |
Total
|
58.523
|
85
|
|
|
|
|
NPRS 2nd week
|
| |
Between groups
|
195.419
|
2
|
97.709
|
76.820
|
0.000
|
| |
Within groups
|
105.569
|
83
|
1.272
|
|
|
| |
Total
|
300.988
|
85
|
|
|
|
|
NPRS 4th week
|
| |
Between groups
|
159.845
|
2
|
79.923
|
87.521
|
0.000
|
| |
Within groups
|
75.794
|
83
|
0.913
|
|
|
| |
Total
|
235.64
|
85
|
|
|
|
|
NPRS 6th week
|
| |
Between groups
|
97.635
|
2
|
48.818
|
63.630
|
0.000
|
| |
Within groups
|
63.679
|
83
|
0.767
|
|
|
| |
Total
|
161.314
|
85
|
|
|
|
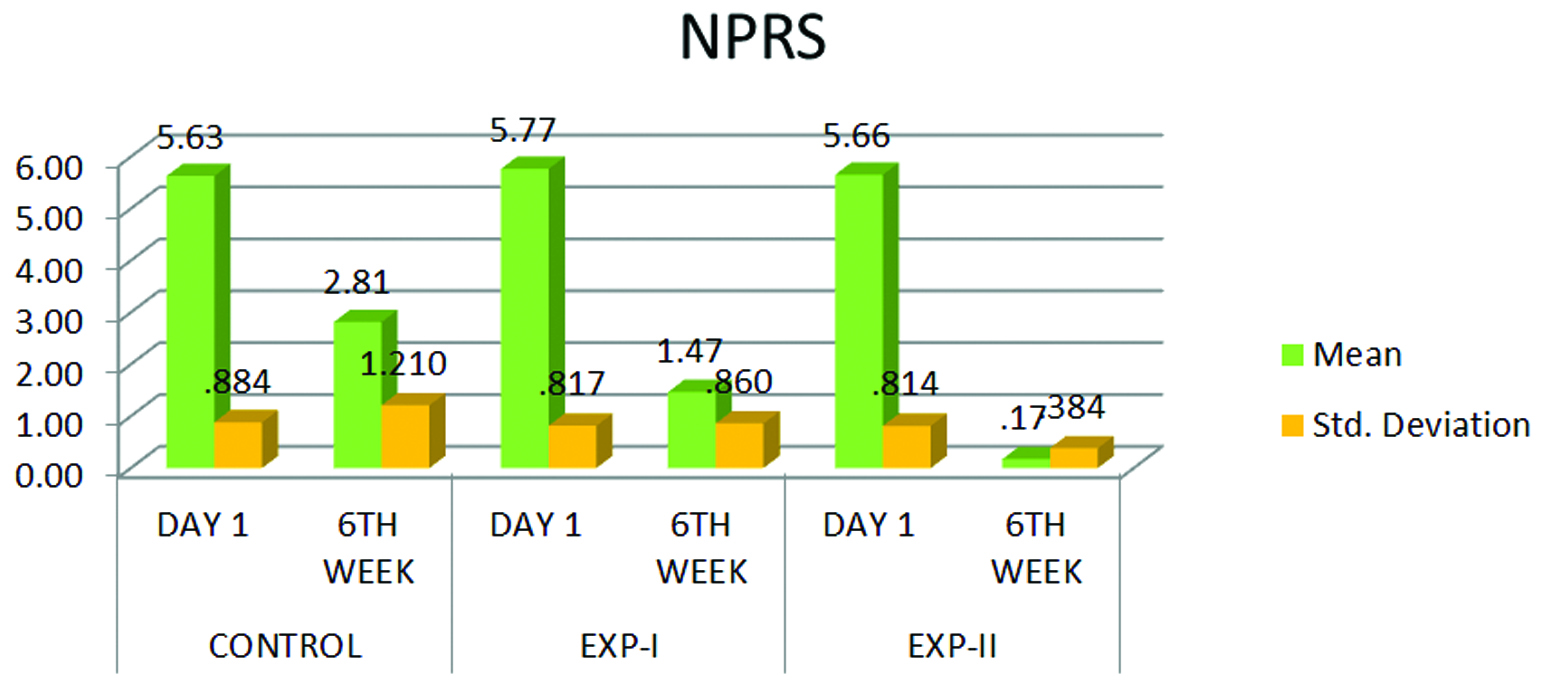
Figure 2: Paired t-test is used to test the significance mean difference in each group.
Table 2: Paired t-test is used to test the effectiveness of day 1 vs week 6 significance mean difference in each group like control, Experimental-1 and Experimental-2 of NPRS.
| |
|
Sum of squares
|
df
|
Mean square
|
F
|
Significance
|
|
MOLBPQ day 1
|
|
|
Between groups
|
232.838
|
2
|
116.419
|
1.517
|
0.225
|
|
|
Within groups
|
6371.499
|
83
|
76.765
|
|
|
|
|
Total
|
6604.337
|
85
|
|
|
|
|
MOLBPQ 2nd week
|
|
|
Between groups
|
866.921
|
2
|
433.461
|
7.361
|
0.001
|
|
|
Within groups
|
4887.834
|
83
|
58.890
|
|
|
|
|
Total
|
5754.756
|
85
|
|
|
|
|
MOLBPQ 4th week
|
|
|
Between groups
|
1140.277
|
2
|
570.139
|
12.99
|
0.000
|
|
|
Within groups
|
3643.862
|
83
|
43.902
|
|
|
|
|
Total
|
4784.14
|
85
|
|
|
|
|
MOLBPQ 6th week
|
|
|
Between groups
|
1781.062
|
2
|
890.531
|
25.470
|
0.000
|
|
|
Within groups
|
2901.972
|
83
|
34.964
|
|
|
|
|
Total
|
4683.035
|
85
|
|
|
|
Modified oswestry low back pain questionnaire There was no significant difference among control group, experimental group 1 and experimental group 2 on day 1 since F-value is 1.517 and its P-value 0.225 is more than 0.05 (Table 3) (Figure 3). A significant difference exists among control group, group 1 and group 2 at week 2, 4, 6 since P-value 0.000 is less than 0.05. Since the paired t-test values of day 1 versus week 6 in control group, experimental group 1 and experimental group 2 are 9.421, 14.960 and 21.495 respectively and mean difference is more in experimental group 2 (Table 4). Hence there is significant improvement in MOLBPQ in the experimental group 2 when compared to experimental group 1 and control group.
Table 3: ANOVA test is used to test the significant mean difference between the groups of MOLBPQ.
| |
|
Sum of squares
|
df
|
Mean square
|
F
|
Significance
|
|
MOLBPQ day 1
|
| |
Between groups
|
232.838
|
2
|
116.419
|
1.517
|
0.225
|
| |
Within groups
|
6371.499
|
83
|
76.765
|
|
|
| |
Total
|
6604.337
|
85
|
|
|
|
|
MOLBPQ 2nd week
|
| |
Between groups
|
866.921
|
2
|
433.461
|
7.361
|
0.001
|
| |
Within groups
|
4887.834
|
83
|
58.890
|
|
|
| |
Total
|
5754.756
|
85
|
|
|
|
|
MOLBPQ 4th week
|
| |
Between groups
|
1140.277
|
2
|
570.139
|
12.987
|
0.000
|
| |
Within groups
|
3643.862
|
83
|
43.902
|
|
|
| |
Total
|
4784.14
|
85
|
|
|
|
|
MOLBPQ 6th week
|
| |
Between groups
|
1781.062
|
2
|
890.531
|
25.470
|
0.000
|
| |
Within groups
|
2901.972
|
83
|
34.964
|
|
|
| |
Total
|
4683.035
|
85
|
|
|
|
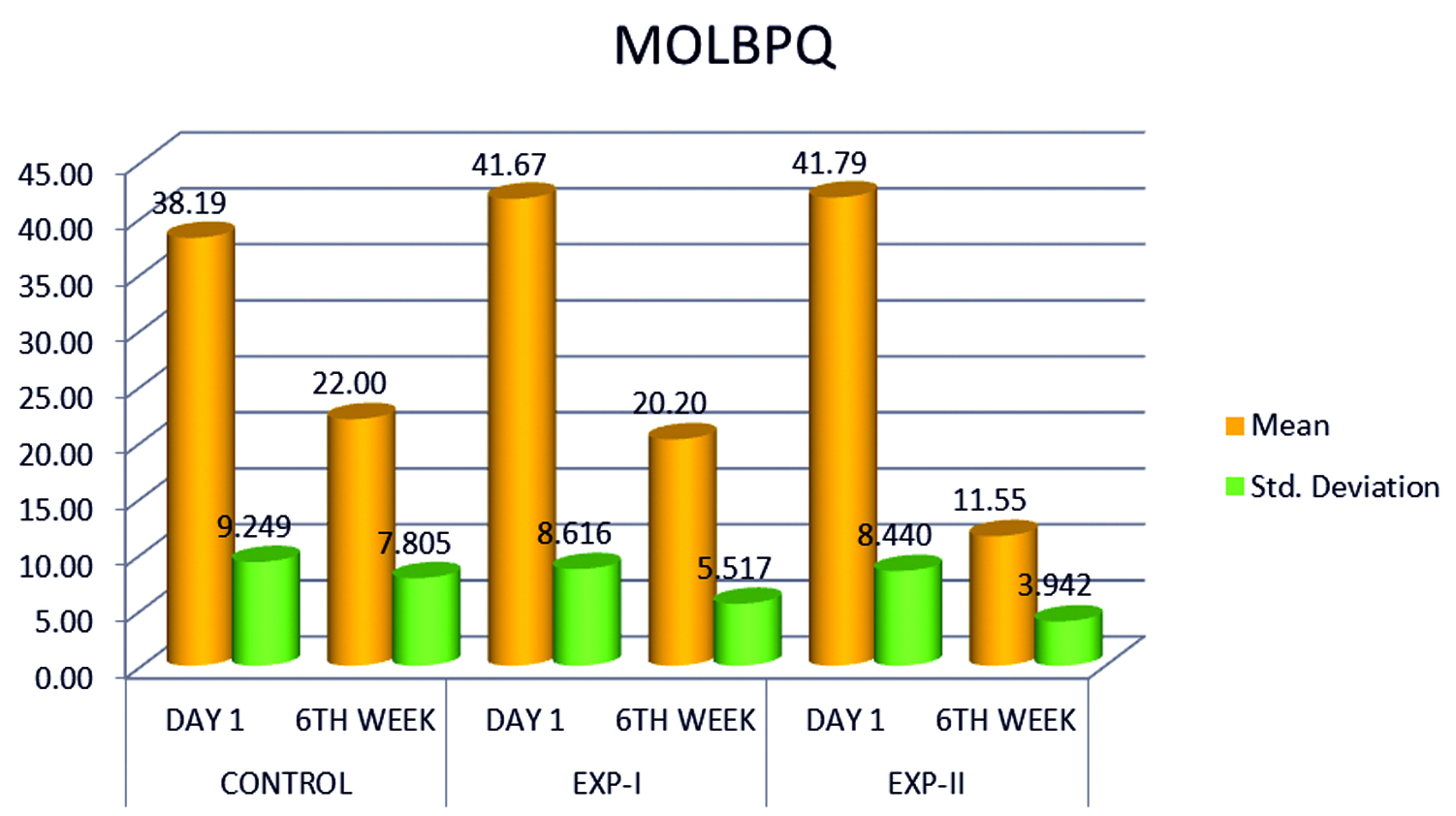
Figure 3: Paired t-test is used to test the significance mean difference in each group.
Table 4: Paired t-test is used to test the effectiveness of day1 Vs week 6 significance mean difference in each group like control, Experimental-1 and Experimental-2 MOLBPQ.
|
Group
|
Mean
|
N
|
Standard
Deviation
|
Standard Error
mean
|
|
Control
|
MOLBPQ day 1
|
38.19
|
27
|
9.249
|
1.78
|
|
|
MOLBPQ 6th week
|
22
|
27
|
7.805
|
1.502
|
|
Experimental 1
|
MOLBPQ day 1
|
41.67
|
30
|
8.616
|
1.573
|
|
|
MOLBPQ 6th week
|
20.2
|
30
|
5.517
|
1.007
|
|
Experimental 2
|
MOLBPQ DAY 1
|
41.79
|
29
|
8.44
|
1.567
|
|
|
MOLBPQ 6th week
|
11.55
|
29
|
3.942
|
0.732
|
|
Group
|
Paired
differences
mean
|
t
|
df
|
Significant
(2-tailed)
|
|
Control
|
MOLBPQ day 1 -
MOLBPQ 6th week
|
16.185
|
9.421
|
26
|
0.000
|
|
Experimental 1
|
MOLBPQ day 1 -
MOLBPQ 6th week
|
21.467
|
14.960
|
29
|
0.000
|
|
Experimental 2
|
MOLBPQ day 1 -
MOLBPQ 6th week
|
30.241
|
21.495
|
28
|
0.000
|
Straight leg raise
There was no significant difference among control group, experimental group 1 and experimental group 2 on day 1 Since F-value is 2.733 and its P-value 0.071 is more than 0.05 (Table 5) (Figure 4). A significant difference exists among control group, group 1 and group 2 at week 2, 4, 6 since P-value 0.000 is less than 0.05. Since the paired t-test values of day 1 versus week 6 in control group, experimental group 1 and experimental group 2 are -12.126, -13.102 and -20.810 respectively and mean difference is more in experimental group 2 (Table 6). Hence there is significant improvement in SLR in the experimental group 2 when compared to experimental group 1 and control group.
Table 5: ANOVA test is used to test the significant mean difference between the groups of SLR.
| |
Sum of squares
|
df
|
Mean square
|
F
|
Significance
|
|
SLR day 1
|
| |
Between groups
|
422.120
|
2
|
211.060
|
2.733
|
0.071
|
| |
Within groups
|
6409.275
|
83
|
77.220
|
|
|
| |
Total
|
6831.395
|
85
|
|
|
|
|
SLR 2nd week
|
| |
Between groups
|
7295.524
|
2
|
3647.762
|
58.871
|
0.000
|
| |
Within groups
|
5142.848
|
83
|
61.962
|
|
|
| |
Total
|
12438.372
|
85
|
|
|
|
|
SLR 4th week
|
| |
Between groups
|
3834.521
|
2
|
1917.260
|
35.992
|
0.000
|
| |
Within groups
|
4421.293
|
83
|
53.269
|
|
|
| |
Total
|
8255.814
|
85
|
|
|
|
|
SLR 6th week
|
| |
Between groups
|
1124.600
|
2
|
562.300
|
13.361
|
0.000
|
| |
Within groups
|
3493.132
|
83
|
42.086
|
|
|
| |
Total
|
4617.733
|
85
|
|
|
|
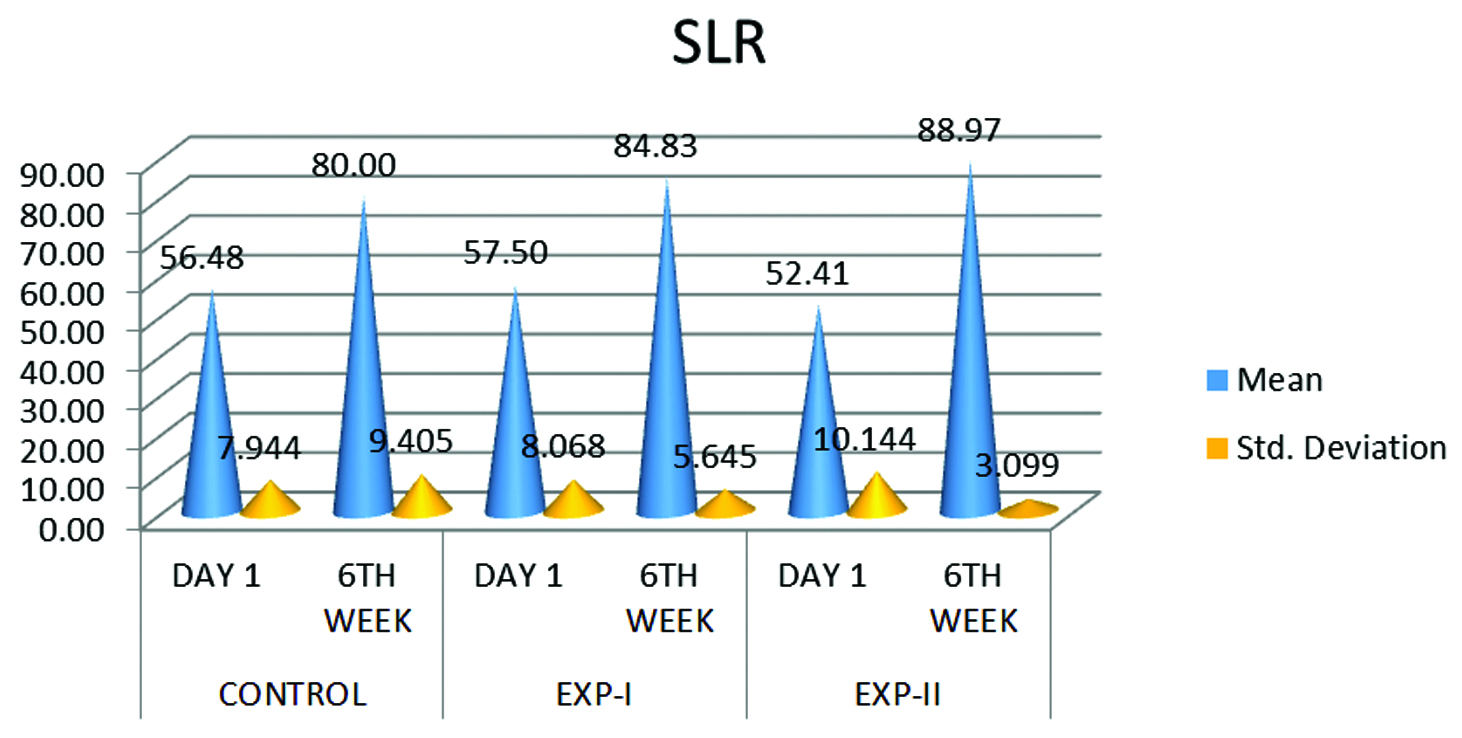
Figure 4: Paired t-test is used to test the significance mean difference in each group.
Table 6: Paired t-test is used to test the effectiveness of day 1 Vs week 6 significance mean difference in each group like control, Experimental-1 and Experimental-2 SLR.
|
Group
|
Mean
|
N
|
Standard
deviation
|
Standard
error
mean
|
|
Control
|
SLR day 1
|
56.48
|
27
|
7.944
|
1.529
|
|
|
SLR 6th week
|
80
|
27
|
9.405
|
1.81
|
|
Experimental 1
|
SLR day 1
|
57.5
|
30
|
8.068
|
1.473
|
|
|
SLR 6th week
|
84.83
|
30
|
5.645
|
1.031
|
|
Experimental 2
|
SLR day 1
|
52.41
|
29
|
10.144
|
1.884
|
|
|
SLR 6th week
|
88.97
|
29
|
3.099
|
0.576
|
|
Group
|
Paired
differences
mean
|
t
|
df
|
Significant
(2-tailed)
|
|
Control
|
SLR day 1 -
SLR 6th week
|
-23.519
|
-12.126
|
26.000
|
0.000
|
|
Experimental 1
|
SLR day 1 -
SLR 6th week
|
-27.333
|
-13.102
|
29.000
|
0.000
|
|
Experimental 2
|
SLR day 1 -
SLR 6th week
|
-36.552
|
-20.810
|
28.000
|
0.000
|
Discussion
The findings of the study indicate that SMWLM three therapist technique as an adjunct to neural mobilization and conventional therapy (experimental group 2) showed significant improvement in pain, functional disability and SLR when compared to neural mobilization with conventional therapy (experimental group 1) and conventional therapy (control group). This supports that both spinal manipulation and neural mobilization techniques have a role in the treatment of lumbar radiculopathy. This is in agreement with Waleed who compared the effect of neural mobilization versus spinal mobilization in patients with radicular chronic low back pain [20]. Spinal mobilization and neural mobilization both were effective in improving the symptoms but spinal mobilization showed an immediate effect. This might be due to correction of positional fault done by SMWLM at the spinal level whereas neural mobilization worked on restoring the mobility of the nerve to its mechanical interface which was compressed due to herniated disc resulting in pain. The minor positional fault might have caused pressure on pain-sensitive structures and nerve roots. In SMWLM, rotation glide was used which might have increased the space of intervertebral for amen by opening intervertebral position and thereby decompressing the nerve roots. This is in agreement with the biomechanical study done by Fujiwara et al. who showed that axial rotation increased intervertebral foramen height and area at the side opposite to the rotation [21]. The neurophysiologic mechanism is another mechanism by which SMWLM has been believed to relieve pain [22].
Experimental group 1 and 2 were treated with neural mobilization technique showed improvement in pain and SLR as neural mobilization has a positive impact on restoring mobility of the nerve and this might have improved neural tissue gliding with respect to its interface [23]. Gladson et al., mentioned that compression of nerve root leads to decreased microcirculation resulting in neural edema and demyelination. The short oscillatory movements in neural mobilization help to reduce neural tissue hypoxia and reduce inflammation. In addition, there is a hypothesis that nerve movement within pain-free variation can help to reduce mechanosensitivity of the nerve [24]. Therefore neural mobilization improves altered circulation to neural tissue and altered axonal transport dynamics by breaking adhesions hence correcting pathophysiology and relieving pain and improving SLR in patients in group 2 and 3.
Although conventional therapy, neural mobilization have an effect in decreasing low back pain, functional disability and improving SLR, however SMWLM as an adjunct to neural mobilization and conventional therapy showed better results than conventional therapy or neural mobilization with conventional therapy. It could be attributed to clear effect of SMWLM that produced greater hypoalgesia than other exercises. It was hypothesized that manipulation inhibits pain at dorsal horn of spinal cord by altering neuroplasticity of the nerve and central sensitization. Spinal mobilization may provide a stimulus that acts as counter-irritant to C fiber-mediated pain [25].
Conclusion
All the three groups showed improvement in pain, functional disability and SLR. SMWLM as an adjunct to neural mobilization and conventional therapy showed significantly better outcomes and was more effective in improving pain, functional disability and SLR when compared to conventional therapy or neural mobilization and conventional therapy.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Murphy DR, Hurwitz EL, Gerrard JK, Clary R. Pain patterns and descriptions in patients with radicular pain: Does the pain necessarily follow a specific dermatome? Chiropr Osteopat. 2009; 17:9.
[2] Nevan G. Baldwin. Lumbar disc disease: The natural history. Neurosurg Focus. 2002; 13(2):1–4.
[3] M Krismer M. van Tulder. Low back pain (nonspecific). Rheumatology. 2007; 21(1):77–91.
[4] Sharma SC, Singh R, Sharma AK, Mittal R. Incidence of low back pain in workage adults in rural North India. Indian J Med Sci. 2003; 57(4):145–147.
[5] Bogduk N. Management of chronic low back pain. Med J Aust. 2004; 180(2):79–83.
[6] Kinkade S. Evaluation and treatment of acute low back pain. American Family Physician. 2007.
[7] Werners R, Pynsent PB, Bulstrode CJ. Randomized trial comparing interferential therapy with motorized lumbar traction and massage in the management of low back pain in a primary care setting. Spine (Phila Pa 1976). 1999; 24(15):1579–1584.
[8] Exelby L. The mulligan concept: Its application in management in spinal conditions. Man Ther. 2002; 7(2):64–70.
[9] Carroll M, Yau J, Rome K, Hing W. Measurement of tibial nerve excursion during ankle joint dorsiflexion in a weight bearing position with ultrasound imaging. J Foot Ankle Res. 2012; 5(5):1–6.
[10] Mulligan BR. Manual therapy. “nags”, “Snags”, “MWMs”, etc 4th edition. Pg:44-45.
[11] Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, et al. A clinical prediction rule to identify patients likely to benefit from spinal manipulation: A validation study. Ann Intern Med. 2004; 141(12):920–928.
[12] Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994; 58(3):387–392.
[13] Stratford PW, Spadoni GF. The reliability, consistency and clinical application of a numerical pain rating scale. Physiothe Can. 2001; 53:88–91.
[14] Gajdosik RL, Bohannon RW. Clinical measurement of range of motion: Review of goniometry emphasizing reliability and validity. Phys Ther. 1987; 67(12):1867–1872.
[15] Fritz JM, George SZ, Delitto A. The role of fear avoidance beliefs in acute low back pain: relationship with current and future disability and work status. Pain. 2001; 94(1):7–15.
[16] John A McCulloch. Macnab's backache; 3rd edition; chapter 13; 408-409.
[17] Jean Olliver. Back Care &Illustrated guide. 3rd edition; chapter 3; 61-117.
[18] Ronald J Schenk, Cherie Jozefczyk, Aric Kopf. A randomized trial comparing intervention in patients with lumbar posterior derangement. J Man Manip Ther. 2003; 11(2):95–102.
[19] Butler SD. Mobilization of the nervous system: tension testing- the lower limbs and trunk. 1991.
[20] El-din Mahmoud WS. Effect of neural mobilization versus spinal manipulation in patients with radicular chronic low back pain. European journal of scientific research. 2015; 131(1):122–132.
[21] Fujiwara A, An HS, Lim TH, Haughton VM. Morphologic changes in the lumbar intervertebral foramen due to flexion-extension, lateral bending, and axial rotation: an in vitro anatomic and biomechanical study. Spine. 2001; 26(8):876–882.
[22] Paungmali A, O'Leary S, Souvlis T, Vicenzino B. Hypoalgaesic and sympathoexcitatory effects of mobilization with movement for lateral epicondyalgia. Phys Ther. 2003; 83(4):374–383.
[23] Sarkari E, Multani NK. Efficacy of neural mobilisation in sciatica. Journal of Exercise Science and Physiotherapy. 2007; 3(2):136–141.
[24] Gladson RB, Taciane SS, Danilo LT, Adriano PC, Alberito RC. Neural mobilization and static stretching in an experimental Sciatica model: An experimental study. Rev Bras Fisioter. 2009; 13(6):493–498.
[25] Perry J, Green A, Singh S, Watson P. A preliminary investigation into the magnitude of effect of lumbar extension exercises and a segmental rotatory manipulation on sympathetic nervous system activity. Man Ther. 2011; 16(2):190–119.