Full Text
Introduction
Hemorrhage is still the commonest cause of maternal mortality in India. Primary postpartum hemorrhage is common but secondary postpartum hemorrhage (PPH) is rare. Secondary PPH has received very little attention probably because of its low incidence and it causes more morbidity than mortality. However severe secondary PPH may sometimes become fatal. The common causes of secondary PPH are retained placenta, endometritis, sub involution of placental bed. Rare causes include pseudoaneurysm, choriocarcinoma, and AV malformations. With newer modalities of treatment, vascular abnormalities are emerging causes of PPH, namely aneurysm, AV malformations and injured vessel. Effective primary management includes use of uterotonic drugs and antibiotics. Failure of conservative management calls for more radical procedures like hypogastric artery ligation or hysterectomy. Ultrasound and angiography have helped to identify women with vascular abnormalities leading to PPH. Uterine artery embolization has been a safe and reliable alternative procedure for PPH that is strongly recommended by various authorities when the women is hemodynamically stable. Failure of treatment with medicine uterine artery embolization necessitates hysterectomy. Secondary PPH beyond the 3rd week after delivery is extremely very rare following LSCS.
A case is reported of uterine artery pseudoaneurysm with secondary PPH, 3 weeks after LSCS and managed successfully with uterine artery embolization.
Case report
A 23 yr old patient (primipara), delivered a 3.25 kg female child by emergency caesarean section 26 days earlier, in a private hospital for failed progression of labor. Ante partum and Intra partum periods were uneventful. She was apparently asymptomatic for first 20 days post operatively. Later she had 2 episodes of severe bleeding per vaginum associated with hypotension and giddiness. Symptomatic treatment was given with uterotonic drugs and IV fluids to which she responded, but there was mild pain in abdomen and mild per vaginal bleeding. She was referred to our institute for further management.
The patient has no history of bleeding disorders, diabetes mellitus, or hypertension. On examination of the patient, she was moderately built with severe pallor, vitals are stable, heart/ lungs are normal. On examination, the abdomen was soft with no palpable mass or tenderness. Caesarean section scar was found to be healthy. On speculum examination of cervix, OS closed with minimal bleeding per vaginum. On vaginal examination, uterus was of 10 weeks size, mobile, no tenderness and fornices were free.
Investigations
1) Blood Investigation: Revealed Hb % 6.5 gm/dl, platelet count normal, bleeding time and clotting time normal. ESR, RFT, LFT and D-DIMER are within normal limits. 1 unit of fresh compatible packed cells blood transfusion was given & broad spectrum antibiotics were started. 2) TVS with color doppler was done and confirmed: a) a postpartum uterus; b) no e/o residual placental tissue in endometrial cavity & endometrial thickness was 8 mm; c) A hypoechoic lesion of size 1.7 x 1.0 cm detected in the Lower uterine segment of uterus, postero inferior to the site of scar (Figure 1). d) Color flow doppler showed Yin & Yang blood flow pattern within the body of pseudoaneurysm (Figure 2A, 2B).

Figure 1: A hypoechoic lesion of size 1.7 x 1.0 cm detected in the LUS region of uterus, postero inferior to scar site, which represented a blood vessel dilated.
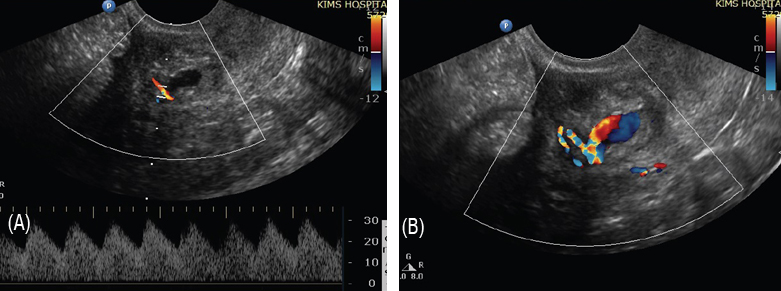
Figure 2A, 2B: Color flow doppler showed ‘Yin & Yang’ blood flow pattern within the body of pseudoaneurysm
e) CT angiogram with non ionic contrast showed right uterine artery of size as 20 x 8 x 7mm with contrast filled out pouching of size 1.7 x 1.0 cm from intramural branch of lower segment of uterus. There was no e/o active leak of contrast. Rest of the artery is normal in course and calibre, suggestive of pseudo aneurysm of intrauterine branch of right uterine artery (Figure 3).
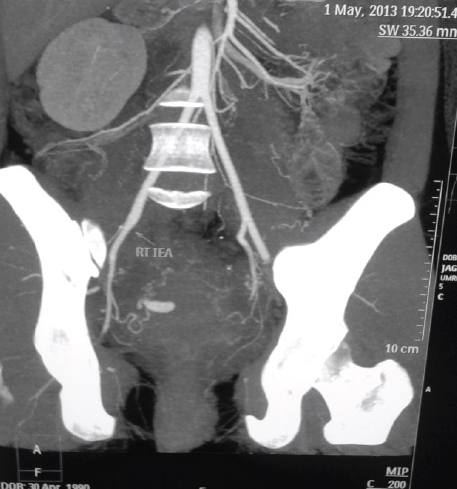
Figure 3: CT angiogram with non ionic contrast showed right uterine artery of size 20 x 8 x 7mm representing a pseudoanaeurysm.
To preserve fertility in this young patient, a trans catheter arterial embolization of this pseudo aneurysm was planned.
Procedure
Endovascular embolization of right uterine artery pseudoaneurysm was done via right femoral trans catheterization, under local anaesthesia and under aseptic precautions. Anaeurysm was selectively cannulated with microcatheter and embolization was done with 25% N-butyl cyanoacrylate & lipoidol glue mixture (Figure 4A, 4B).
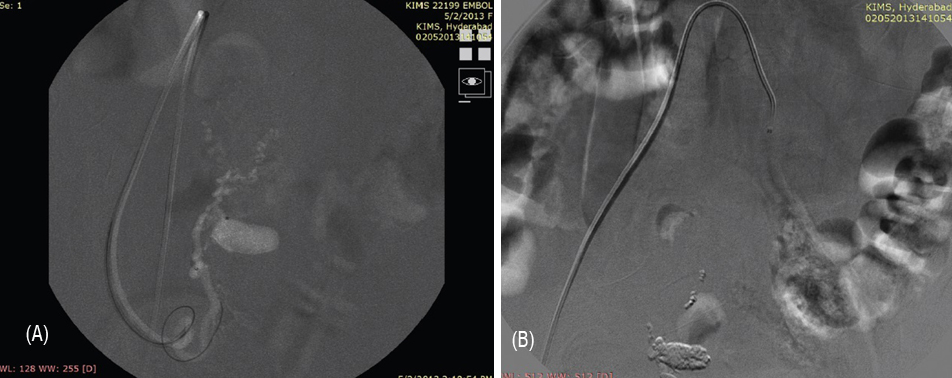
Figure 4A, 4B: Post procedure angiogram showing complete obliteration of pseudo anaeurysm from circulation.
Discussion
Pseudoaneurysm is an extra-luminal collection of blood with turbulent flow that communicates with parent vessel through a defect in arterial wall. It is a rare but life threatening complication of uterine surgery, especially in caesarean section. It results in secondary postpartum hemorrhage which is defined as haemorrhage occurring between 24 hrs and 6-12 wks postpartum.
Etiology: Aneurysm can occur following: A) Surgery: 1) Caesarean Section, 2) Pelvic surgery – Hysterectomy, myomectomy, Radical onco surgery, 3) Dilatation & curettage, 4) After oocyte retrieval in IVF; B) Uncomplicated vaginal delivery; C) Trauma; D) Infection; E) Neoplasms
Etiopathogenesis: During the surgical procedures, when the vessel is either lacerated/ ruptured leads to hematoma formation and central liquefaction that leaves a cavity with turbulent blood flow, resulting in persistent communication between artery and hematoma leading to pseudo aneurysm. The absence of a 3- layer arterial wall lining the pseudo aneurysm differentiates it from a true aneurysm.
Differential diagnosis
1) Retained products of gestation 2) Endometritis 3) Subinvolution of placental bed 4) Choriocarcinoma 5) Arterio venous malformations; Diagnosis: 1) Grey scale ultrasound - A hypoechoic lesion associated with uterine incision; 2) Color doppler sonography - TO & FRO sign in the neck of pseudoaneurysm and YIN – YANG sign in the body of pseudoaneurysm. AVM’ s are characterized by marked aliasing on color flow doppler and arterialized venous flow on spectral doppler. Sensitivity is 95%; 3) CT-angiography – confirms & rules out other causes.
Clinical features include asymptomatic, may thrombose or may lead to distal painful embolization. Severe vaginal bleeding or secondary PPH is the most common presentation. Pain abdomen, supra pubic pain are the major symptoms, death may occur if ruptured. The risk of rupture is proportional to the size and intramural pressure. In the past, majority are treated with hysterectomy.
In the recent years, uterine artery embolization has become the accepted method of treatment for uterine artery pseudoaneurysm in hemodynamically stable patients. Angiographic embolization has the advantages of 1) Decreased morbidity. 2) Ability to localize the bleeding site. 3) More distal occlusion than surgical ligation. 4) Avoids general anesthesia. 5) Preservation of future fertility compared with hysterectomy. 6) Repeat embolization can be easily performed if required.
In 1979, Brown et al., reported a first case of selective arterial embolization used successfully to treat an extra uterine pelvic hematoma after three failed surgical attempts to control bleeding [1]. In a series of women with pseudoaneurysm, Rosenthal et al. observed angiographic arterial embolization to be the most useful clinical tool in management of post OP vaginal hemorrhage [2]. Najundan has reported a similar case of secondary PPH on the 19th day after caeserean section, which was treated by embolisation [3]. Cooper et al. also reported a case of uterine artery pseudo aneurysm presenting as delayed PPH requiring B/L embolisation [4]. Henrich et al. described the sonographic diagnosis and treatement [4].
Conclusion
Injuries to the vessels are more likely during a caesarean section which could subsequently give rise to pseudoaneurysm. Doppler ultrasonography and angiography are useful techniques to diagnose this condition. Selective embolization of an affected vessel could be done with bleeding arrested instantaneously. Being a minimally invasive procedure and causing no risks to mother, embolization should be offered whenever and wherever feasible. With newer modalities of treatment available, hysterectomy for PPH should be the last resort.
Conflicts of interest
Authors declare no conflicts of interest.
References
1. Brown BJ, Heaston DK, Poulson AM, Gabert HA, Mineau DE, et al. Uncontrollable postpartum bleeding: a new approach to hemostasis through angiographic arterial embolization. Obstet Gynecol. 1979; 54(3):361-365.
2. Rosenthal DM, Colapinto R. Angiographic arterial embolization in the management of postoperative vaginal haemorrhage. Am J Obstet Gynecol. 1985; 151(2):227-231.
3. Najundan P, Rohilla M, Raveendran A. Pseudoaneurysm of Uterine Artery: A Rare Cause of Secondary Postpartum Hemorrhage, Managed with Uterine Artery Embolisation. J Clin Imaging Sci. 2011; 1:14.
4. Cooper BC, Hocking–Brown M, Sorosky JI, Hansen WF. Pseudoaneurysm of the Uterine Artery Requiring Bilateral Uterine Artery Embolization. J Perinatol. 2004; 24:560-562.
5. Henrich W, Fuchs I, Luttkus A, Hauptmann S, Dudenhausen JW. Pseudoaneurysm of the uterine artery after cesarean delivery: sonographic diagnosis and treatment. J Ultrasound Med. 2002; 21(12):1431-1434.